American writer, David Auerbach, said it best: “In Wine there is Wisdom. In Beer there is Freedom. In Water there is Bacteria”. More than just a catchy phrase, it is also true, well at least about water. This article highlights one of the lesser-known waterborne bacteria: Legionella.
What is Legionella?
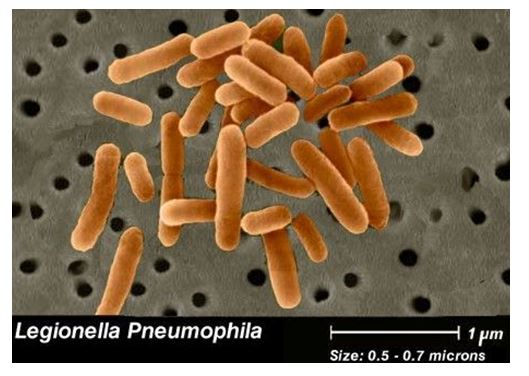
Legionellais a pathogenic (disease-causing) group of bacteria found naturally in freshwater environments. It thrives in warmer waters as high as 50oC. It can even invade man-made systems such as cooling towers, swimming pools, hot-water showers and faucets, ice-making machines, decorative fountains, hot water tanks and heaters, hot tubs, saunas and whirlpool spas.
The bacterium can survive for months in tap and distilled water. Legionella appears to be more resistant to chlorine than the well-known food-borne pathogen, Escherichia coli.
At least 40 species of Legionella have been shown to cause disease, but the most prominent pathogenic species is Legionella pneumophilia.
History
The bacterium can survive for months in tap and distilled water. Legionella appears to be more resistant to chlorine than the well-known food-borne pathogen, Escherichia coli.
At least 40 species of Legionella have been shown to cause disease, but the most prominent pathogenic species is Legionella pneumophilia.
How is Legionella transmitted?
Legionella bacteria typically does not spread directly between people – it is not contagious.
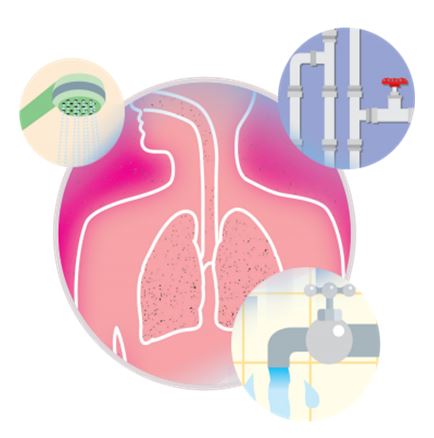
Transmission of the Legionella bacteria occurs when microscopic airborne droplets of water or mist that contains elevated levels of bacteria is inhaled. In addition, droplets and particles may accidently enter the respiratory system rather than the digestive system during the swallowing process (aspiration).
Legionella bacteria can affect anyone, including healthy individuals. However, Legionella is an “opportunistic” bacteria that usually affects individuals with underlying illnesses or conditions. Individuals particularly at risk include those with respiratory disease, diabetes (as well as dialysis patients), cancer, weakened immune systems, organ transplant patients, the elderly, and heavy smokers or drinkers.
What are the effects of exposure to Legionella?
Legionella is the causative agent of legionellosis, a term coined for all diseases caused by this type of bacteria. Legionellosis includes two distinct forms: Legionnaires’ disease and Pontiac Fever.
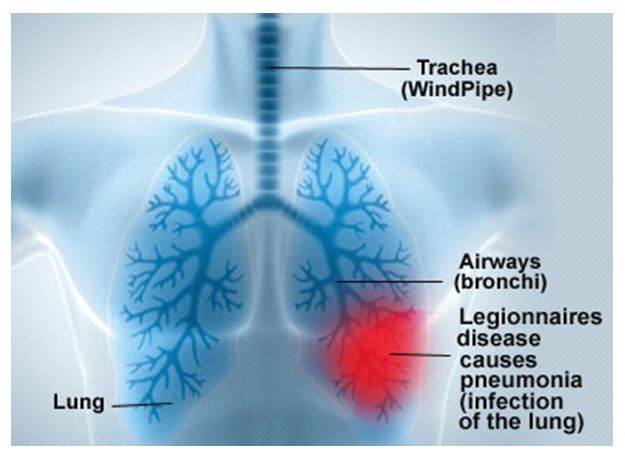
Legionnaires’ disease is a severe form of pneumonia. The incubation period is 2 to 10 days and rarely up to 20 days. Legionnaires’ disease usually lasts for weeks, with a fairly high mortality rate. Legionnaires’ disease is often initially characterized by anorexia, malaise, lethargy and a mild unproductive cough. Though most symptoms are non-specific, they include: Loss of strength (asthenia), High fever, Headache, Chills, Muscle pain, Difficulty breathing, Chest pain, Diarrhea, Vomiting, Nausea, Central nervous system manifestations, such as confusion and delirium, and even Renal failure (World Health Organization, 2007).
Pontiac fever refers to an acute flu-like illness that is milder than Legionnaires’ disease, self-limiting (resolving itself without treatment) and non-fatal. The incubation period is 5 hours to 3 days (most commonly between 24 to 48 hours). Pontiac fever usually last for 2-5 days. Typical symptoms include: Influenza-like illness (moderate to severe), Loss of strength (asthenia), tiredness, High fever and chills, Muscle pain (myalgia), Headache, Joint pain (arthralgia), Diarrhea, Nausea, Vomiting, Difficult breathing (dyspnoea) and dry cough (World Health Organization, 2007).
Prevalence
A report from the Center for Disease Control (CDC) revealed that from 2000 to 2014, the rate of reported cases of legionellosis, increased nearly fourfold. CDC Director, Mr. Tom Frieden, reported that “People are unnecessarily and avoidably getting sick and dying from preventable infections. And the cases carry a high price tag: The annual cost of treating Legionnaire’s disease, based on hospital claims, is about $434 million”.
The CDC analyzed outbreaks it had investigated from 2000 to 2014 that involved 415 cases, including 65 deaths. Most of the outbreaks were in buildings with large or complex water systems, such as hotels, hospitals and long-term-care facilities. About half of outbreaks examined were the result of a single failure, such as a broken disinfection system or human error. The most common sources of the bacteria were water in showers, cooling towers and hot tubs.
Treatment & Prevention
There are no vaccines for preventing legionellosis. Medical treatment for Legionnaires’ disease requires the use of antibiotics. The best method of prevention is to eliminate water conditions that allow the Legionella bacteria to thrive and to prevent the spreading of contaminated aerosols.
Measures include good maintenance of equipment and devices, application of physical (temperature) and/or chemical measures (biocides) to minimize growth. Some examples include:
- Regular maintenance, cleaning and disinfection of cooling towers;
- Maintaining an adequate level of a biocide (e.g. chlorine) in major water distribution systems;
- Keeping the hot water at 60°C and the cold below 20°C or alternatively treating them with a suitable biocide to limit growth;
- Keeping hot and cold water systems clean and free of scale in order to reduce stagnation and
- Flushing unused taps in buildings on a weekly basis.
Applying such controls can greatly reduce the risk of Legionella contamination and prevent the occurrence of outbreaks. Don’t allow these tiny bacteria to turn the tables and put you in hot water.
Contact CARIRI’s Environmental Microbiology Laboratory for more information on Legionella Evaluations at emicro@cariri.com or 285-5050 ext 3504/3509/3512.

